Advancing Precision in AMD Detection – Part 1
The ZEISS CIRRUS is invaluable in helping to detect and diagnose glaucoma, macular degeneration, and whole host of retinal pathologies, says optometrist Robert Foulds.
Robert Foulds is a consultant optometrist and partner at Donovan Smith Opticians, a Brighouse-based practice that first opened 60 years ago. Robert runs the practice with his wife, Carol, a dispensing optician, and daughter Molly, an optometrist. Family values are key to Donovan Smith’s standing in the community – as is its investment in the latest and best optical equipment. A longtime user of ZEISS instruments and systems, Robert tells The New Optometrist how the CIRRUS 6000 OCT has transformed the way he diagnoses and detects macular degeneration, glaucoma, and other retinal pathologies, and how he is preparing enthusiastically to bring the device’s OCT-A and RPE analysis capabilities into play.
Why did you choose the ZEISS CIRRUS OCT for your practice?
We were one of the first practices in the UK to get OCT. Some of my colleagues were quite cynical at the time, thinking that a) we wouldn’t use it, and b) patients wouldn’t fund it because it’s outside the remit of the health service. But we worked closely with the manufacture and went ahead with it. The ZEISS CIRRUS is our third OCT now, and it’s been fantastic for us.
We selected the CIRRUS because we wanted to use the ZEISS CLARUS 500 ultrawide fundus imaging system alongside it. To these instruments we’ve added the Humphrey Field Analyzer and we link all three with ZEISS FORUM ophthalmology software, which really makes for a slick facility in the consulting room. We’re able to see results from all three instruments and meld them together. Features such as the guided progression analysis to help detect and monitor glaucoma are just superb using FORUM. It’s very user friendly, so it’s easy for the optometrist to get into the images, explain them to the patient, and integrate the results and longitudinal data with those from the other ZEISS instruments.
We’re a three-optometrist practice, and we’re quite clinically based. We’ve built up a good reputation in the area with doctors and eye consultants – and obviously our patients – for offering a long and thorough eye examination. I couldn’t actually work without OCT now. It has a good take-up among patients and has proved indispensable in helping to diagnose and detect glaucoma, macular degeneration, and a whole host of retinal pathologies.
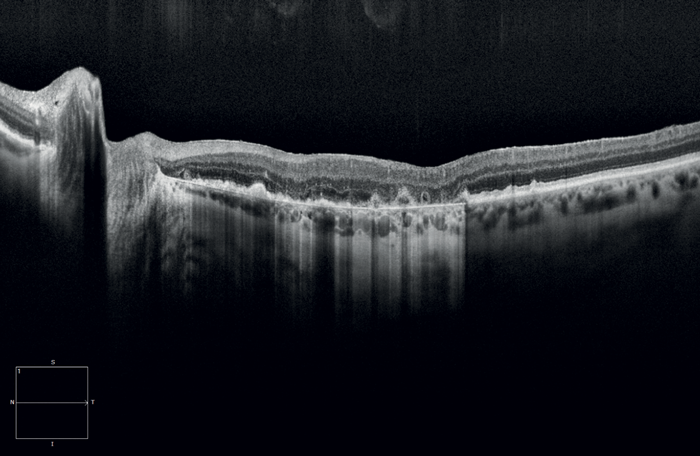
When a patient has a drop in vision, we like to try and investigate exactly why that’s happening. But when that patient is mature in years and they’ve got moderate to dense cataracts, sometimes you can’t see the back of the eye very well. The CIRRUS is invaluable here, because it will check the general health of the eye; if the macular is perfectly healthy for example, cataract surgery is going to be of benefit. But quite often you’ll pick up a retinal lesion such as dry or – God forbid – wet macular degeneration, and that has to be looked at as a priority before cataract surgery takes place.
The CIRRUS is really good here because it helps us detect whether that macular degeneration is wet – if there’s intraretinal fluid, subretinal fluid, sub-retinal pigment epithelium (sub-RPE) fluid – or whether it is dry, which, in the case of geographic atrophy (GA), hasn’t been amenable to any form of treatment to date.
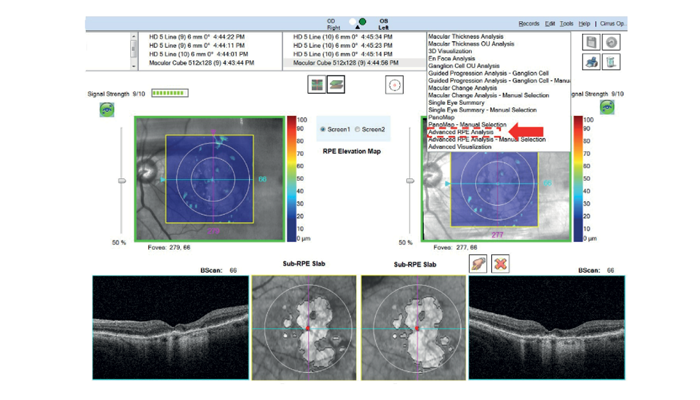
On the subject of RPE, this is another reason we chose the CIRRUS – it exclusively features Advanced RPE Analysis software, which we’re about to start using extensively following the imminent availability of Dry AMD therapies. It has proprietary algorithms that provide a whole host of invaluable metrics. These therapies will finally offer those patients with Geographic Atrophy, hope. We’re also about to install AngioPlex, OCT-angiography on the instrument to complement the RPE Analysis.
What would the ability to improve diagnosis, management, and referral of GA patients mean for you?
As with the wet AMD patients, if there is treatment out there for GA, it means we can attach the scans to our referral on the email portal, which would go urgently to the macular clinic. The referral is triaged very quickly, and we can see that the patient has been contacted to make an appointment either that same day or in the next few days. Or, if the consultant doesn’t feel it is an urgent case, then within the next weeks or months. But it means the facility is there for somebody to be seen in the macular clinic and receives the appropriate treatment/therapies, should it be deemed necessary.
You mention that you’re introducing Advanced RPE analysis and ZEISS AngioPlex OCT-A. What do you expect from these capabilities?
Well, we always had Advanced RPE Analysis, it’s built-in to every CIRRUS 5000 and 6000 device, but with Dry AMD therapies on the horizon it becomes invaluable for GA assessment. It would also be extremely useful to see the capillary networks in much more detail underneath the macular. We should be able to look in depth at the capillary networks and the retinal perfusion using OCT-A, the latter without the need for a fluorescein angiogram, which we can’t do in an optometric practice anyway.
With geographic atrophy, at the moment, all we do on a structural OCT scan is look for what we call the waterfall effect, where the light is effusing through the retina because the RPE cells are just not there in the numbers that they’re supposed to be. I expect the RPE analysis to give us a much more in-depth overview of that layer in the retina, with visit comparison metrics that will help us determine current progression, as the analysis can also be run on all my legacy data.
Even if there wasn’t a successful treatment out there, the Advanced RPE Analysis shows why somebody’s vision is deteriorating, you can communicate this to the patient in a palatable manner by showing them the images on screen. The 3 and 5mm circles on the fundus image can be related to dinner plates, with 3 (for example) Digestive Biscuits (of course there are other flavours) located on the peripheral edges. As the Disease progresses the biscuits (Lesions) sadly get closer to the centre, and eventually overlap where our patient’s central vision would be severely compromised/if not lost. I always try to reassure patients with severe maculopathy that they’re not going to end up in a world of complete darkness. If you can show patients with the Advanced RPE Analysis that only the very central macular area is affected and visually illustrate that the rest of the retina is in good health, they can be reassured that they’re going to maintain good navigational vision and not be in that world of darkness.
So, I expect to be able to look in depth at the capillary networks and the retinal perfusion using OCT-A, and use Advanced RPE analysis to look for pigment epithelial cell loss.
The next time we talk, you’ll have first-hand experience of utilizing OCT-A in practice…
Yes, ZEISS will be coming into our practice to install AngioPlex and give us a full introduction to OCT-Angiography, with a refresher on the Advanced RPE Analysis in light of these new therapies. I look forward to giving you my impressions of using these tools in unison, in practice.
The New Optometrist Newsletter
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Most Popular
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here