Topical Cannabinoids and Ocular Pain Relief
Endocannabinoid system (ECS) modulation has been observed to have a wide range of potential therapeutic benefits for multiple disorders, including ocular pain
Though a number of different treatment options exist, safe and effective management of ocular pain remains a challenge. This year marks 60 years since the identification of the structure of two major cannabinoids – THC and CBD (1). This advance set in motion a series of discoveries leading to identification of the endocannabinoid system (ECS). This intricate signaling ystem of molecules, receptors, and enzymes is present in nearly all organs, including the eye, and ECS modulation has been observed to have a wide range of potential therapeutic benefits for multiple disorders, including ocular pain (2). Coupled with advances in drug delivery systems, ECS modulators have the potential to provide localized ophthalmic drug delivery that avoids systemic effects.
Both topical and systemic analgesics can effectively relieve acute ocular pain, but they have marked limitations in terms of their safety profile (3). For example, topical anesthetics and non-steroidal anti-inflammatory drugs (NSAIDs) may delay epithelial healing, whereas systemic gabapentinoids and opioids have been shown to lead to sedation and respiratory depression.
Treatment of chronic ocular pain can present an even greater challenge. This pain may accompany a chronic disease state, such as dry eye disease (DED) or diabetes, and though treatment of the underlying disease is essential, neuronal sensitization can still persist even when the disease is brought under control. Treatment options for chronic neuropathic pain include oral gabapentinoids, opioids, and tricyclic antidepressants. However, their efficacy is limited and the side effects may not be acceptable.
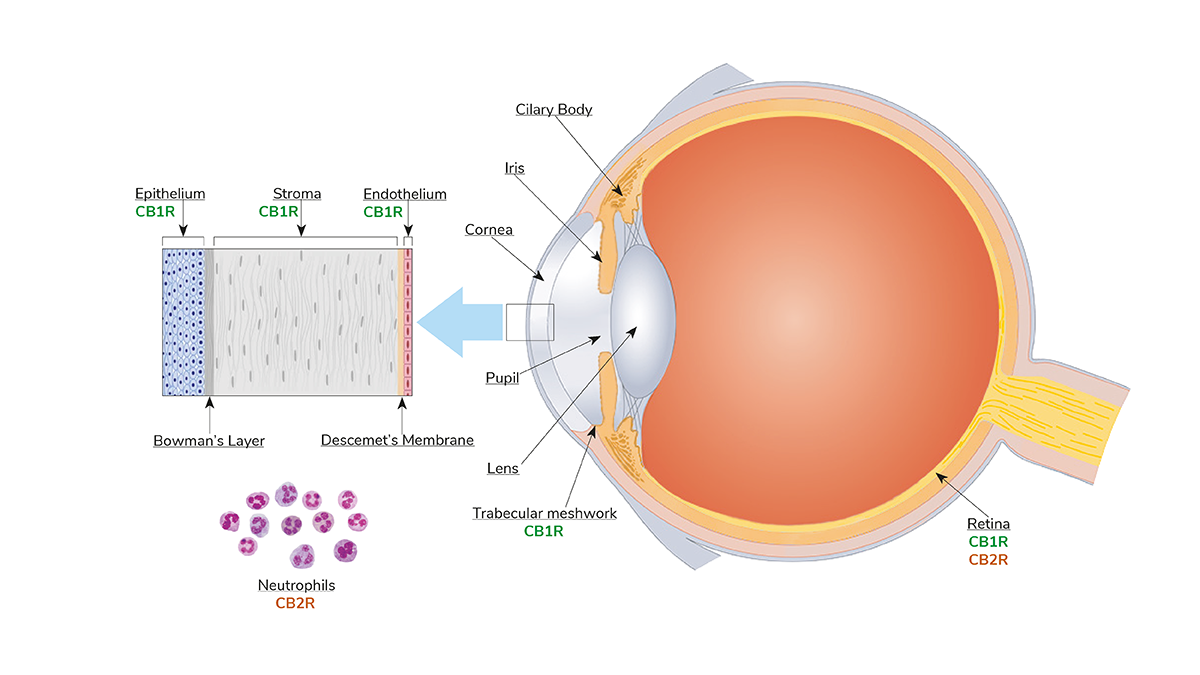
There are three essential components of the ocular ECS: receptors, endogenous cannabinoids, and enzymes responsible for synthesis and degradation of receptors and cannabinoids. Acting to regulate pain transmission, cannabinoid 1 receptor (CB1R) has been identified throughout ocular tissues, whereas the cannabinoid 2 receptor (CB2R) is primarily localized to the surface of immune cells (3). Since ocular inflammation can result in both acute and chronic pain, the anti-inflammatory actions of CB2R modulation can have an indirect effect on improving ocular comfort. Reducing the release of noxious inflammatory mediators helps ameliorate acute pain, and prevention of neuronal sensitization by these mediators reduces the possibility of developing chronic neuropathic pain.
Since pain and inflammation often accompany DED, topical cannabinoids could also represent an important therapeutic approach to this condition. Because CB1R is present on the corneal epithelium, topical cannabinoids can easily access a desiccated epithelium – which can be a source of both acute and chronic ocular pain for DED patients – providing significant pain relief.
Interestingly, CB1R is also expressed in neurons innervating the lacrimal gland. Usually the expression is low, but this expression increases during DED-associated inflammation. McDowell et. al highlighted how CB1R activation reduces sensitization of lacrimal gland nerves, potentially reducing chronic neurotrophic pain (4). Tran et. al also demonstrated improvement in corneal fluorescence, and reduction of corneal and conjunctival inflammation after topical application of cannabinoids in experimentally induced dry eye models (5).
Other methods of ECS modulation are currently under investigation. One uses modulators that increase the binding affinity of cannabinoids to the receptors, allowing for a smaller dose of cannabinoid to achieve the desired effect; another method uses enzyme inhibitors that increase levels of endocannabinoids by inhibiting the actions of enzymes that degrade them. Treatment with enzyme inhibitors has been shown to reduce pain and inflammation in several preclinical models, including for chronic neuropathic pain (3).
There are challenges though; ECS modulators are hydrophobic, so the potential bottleneck of ocular penetration and bioavailability needs to be considered; here, nanotechnology-based drug delivery methods may prove useful.
The ubiquitous presence of the endocannabinoid system in ocular tissues, its role in ocular analgesia, and its demonstrated responsiveness to topical modulators represent a unique opportunity to continue developing a novel class of ECS ocular pain relief medications. These medications could either be used alone or in conjunction with other ocular analgesics to optimize ocular comfort, relieving both acute and chronic pain for patients.
References
- V DiMarzo et al., “The endocannabinoid system and its therapeutic exploitation,” Nature Reviews Drug Discovery, 3, 771 (2004). PMID: 15340387.
- JD Lafreniere, MEM Kelly, “Potential for endocannabinoid system modulation in ocular pain and inflammation: filling the gaps in current pharmacological options,” Neuronal Signaling, 2, 4 (2018). PMID: 32714590.
- JD Lafreniere et al., “Topical analgesics for acute corneal pain: current options and emerging therapeutics,” J Cataract Refract Surg, 49, 1160 (2023). PMID: 37232414.
- TS McDowell et al., “CB1 cannabinoid receptor agonist prevents NGF-induced sensitization of TRPV1 in sensory neurons,” Meurosci Lett, 551, 34 (2013). PMID: 23850608.
- BN Tran et al., “Topical Application of Cannabinoid-Ligands Ameliorates Experimental Dry-Eye Disease,” Ocul Surf, 23, 131 (2022). PMID: 34922011.
The New Optometrist Newsletter
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Most Popular
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here