Air Pollution and Eye Health: The “Unknown Unknowns”
New study investigates air pollution’s links to posterior segment ocular diseases
The images in June 2023 of the New York cityscape shrouded in a sepia-coloured blanket of smoke – a by-product of over 400 drifting Canadian wildfires – marked one of the worst days of air pollution in recent US history. Reports carried headlines straight from dystopian fiction – e.g., “smoke apocalypse” (1) – and centered on incidents caused by the sudden drop in air quality, such as the actress Jodie Comer abruptly halting a Broadway performance because she was struggling to breathe (2).
Amid stricter global regulations on carbon emissions, air pollution still accounts for around 11.65 percent of global deaths, and remains one of the leading factors of disease burden (3). Government regulations – such as the UK’s Clean Air (Human Rights) Bill (4) – tend to focus on breathing issues, such as asthma and chronic obstructive pulmonary disease, but many diseases are linked to air quality. Stroke, cardiovascular diseases, trachea, bronchus and lung cancers, autoimmune and intestinal diseases, and even Alzheimer’s disease have all been associated with air pollution by the World Health Organization (WHO) (5).
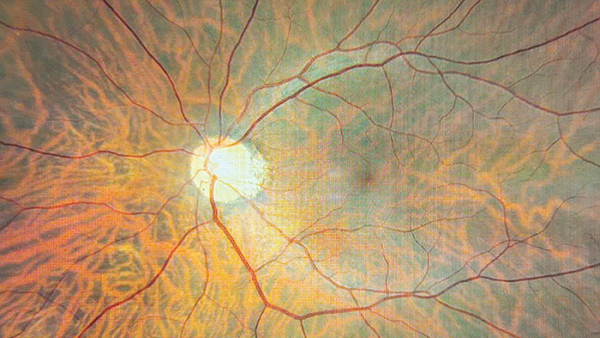
Now, a study in the Journal of Clinical Medicine (6) has reviewed recent medical literature to determine ambient air pollution’s links to vision-threatening posterior segment ocular diseases. Andrzej Grzybowski, Professor of Ophthalmology at the University of Warmia and Mazury, Poland, and one of the study’s main authors, explains that air pollution’s impact on ocular health is poorly perceived. “As ophthalmologists, when we think about air pollution, we usually refer to dry eye syndrome, as the ocular surface disorder.” Of course, the anterior segment of the eye comes into direct contact with the external environment; however, emerging evidence suggests that the posterior segment of the eye is similarly vulnerable to the health effects of polluted air.
Grzybowski contends that better technologies and more standardized methods to track air pollutant levels could become cost-effective preventatives for ocular diseases. We need to have “more and better-evidenced studies,” he says, noting that, in cases such as central retinal artery occlusion (CRAO), there are only a few available studies so far.
To quantify air pollution, the new study measured particulate matter, with PM2.5 referring to particles with a ≤2.5 μm diameter and PM10 referring to particles with a ≤10 μm diameter. Although both these particle sizes can be inhaled and enter the lungs, PM2.5 can also enter the bloodstream. Grzybowski says, “We showed significant associations between PM2.5 and glaucoma, including primary open-angle, primary angle-closure, and normal-tension glaucoma. An increased risk of AMD was linked to increased exposure to PM2.5, NO2, and CO.” He continues, “Single studies suggested that increased exposure to PM2.5 and PM10 is associated with diabetic retinopathy; THC and NMHC increased the risk of retinal vein occlusion; and CO, NO2, and PM10 are linked to an increased risk of CRAO.”
Toxic air pollutants can be identified as a potential modifiable risk factor for visual impairment, particularly posterior segment ocular diseases, the study concludes. But environmental cleaning can take decades, slowing down efforts to minimize the adverse effects of toxic components in the air. “We need to learn more – first, about the pathophysiology of these influences… and the different disorders that might be aggravated by air pollution is not closed,” says Grzybowski. “This is the area of unknown unknowns.”
There is a glimmer of hope, however – the topic is growing in importance. “We will certainly learn more about it in the future – hopefully not only in the context of the increasing number of disorders related to air pollution, but also in terms of minimizing its harmful effects to ocular health,” explains Grzybowski. This is “a complex issue that requires collaborative efforts on a global scale,” he adds.
This article first appeared in The Ophthalmologist
References
- New York Magazine, “How long is the smoke in New York going to last?” (2023). Available at: nym.ag/3qBrKRv.
- BBC News, “Jodie Comer: Prima Facie star halts Broadway show due to wildfire smoke,” (2023). Available at: bbc.in/3X0wmgl.
- CJ Murray et al, “Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019,” The Lancet, 396, 1223 (2020). PMID: 33069327.
- UK Parliament, “Clean Air Bill (Human Rights) Bill” (2023). Available at: bit.ly/43UpIKO.
- World Health Organization, Household Air Pollution (2022). Available at: bit.ly/43VlNNN.
- A Markeviciute et al., “A Review of Ambient Air Pollution as a Risk Factor for Posterior Segment Ocular Diseases,” Journal of Clinical Medicine, 12, 3843 (2023). PMID: 37298038.
The New Optometrist Newsletter
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Most Popular
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here