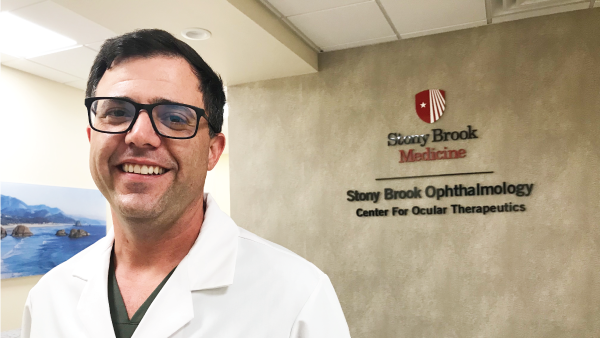
A Whole Body Approach to Seasonal Dry Eye Flares
Why it is crucial to get ahead of seasonal symptoms in dry eye patients
As our attention turns to warmer clothes, football, and all things pumpkin spice (or not), it’s also time to start preparing chronic dry eye patients for seasonal flares. It is crucial to get ahead of symptoms because we know that by the time eyes feel dry, it’s very likely some inflammatory damage has already occurred. So, I take a proactive approach to making sure my dry eye patients are armed and ready for winter.
Indoor air
Seasonal changes trigger flares for a number of reasons, a primary one being indoor air. As we spend more time inside with the heat on, the humidity and temperature of the environment is altered. I tell patients that corneas are sensitive to temperature, as well as humidity and even barometric pressure. Patients with many types of inflammatory conditions describe seasonal flares, and dry eye is no different (1). I suggest patients start using a humidifier, placed by their workstation and/or bed. While we cannot “drink” dry eye away, it is important to stay hydrated and so I remind my patients to keep drinking water, or else add a warm herbal tea in place of the summer water bottle. I remind patients with incomplete lid seal to get those eyes covered or closed at night. Great options for incomplete lid seal include Sleep Tite Sleep Rite shields, Optase A ointment, or Ivizia night gel with a wrap-style sleep mask.
Vitamins and nutraceuticals
It’s also a good time to do a "gut check" and make sure that the patient’s diet is under control. Dietary changes can take three to four months to really kick in, so I urge patients to start or restart nutraceuticals to help support ocular health and maintain tear film homeostasis. I recommend HydroEye formulated with gamma linoleic acid (GLA) (ScienceBased Health), a fatty acid derived from black currant seed oil. I find my patients are very responsive to nutraceuticals, and they love that they can take something that helps from the inside out. GLA is backed by rigorous research showing that it stimulates tear production, in addition to lowering inflammation and improving dry eye symptoms (2-8). HydroEye has been specifically validated in a randomized, controlled clinical trial (9).
I also recommend vitamin D supplements in the winter, as a deficiency can lead to dry eye. A study from Sweden (nearly the same latitude as where I live), showed that my patients would have to be outside for 6.5 hours to get enough vitamin D! (10)
Eye drops and hygiene
If patients let their topical eye drop therapy slip, I encourage them to start back up to be prepared for winter. Topical immunomodulators, like cyclosporine or lifitegrast, can take weeks to months to start working, so it’s time now to get back on that dosing twice a day.
Patients also need to stay on top of their lid hygiene. We know that any concurrent blepharitis, whether it be Demodex or staph, must be kept under control. That could mean daily lid scrubs or the topical drop lotilaner ophthalmic solution (Xdemvy, Tarsus). Preparing ahead of time and getting back on home therapy is a great way to make sure patients are ready for winter. I remind them to be consistent with supportive artificial tears; I favor the iVIZIA line, and Refresh Optiva Mega-3, Relieva, and Digital.
Eyes are not the whole patient
As I say to patients, our eyeballs aren’t “floating around in space;” they are covered with and surrounded by skin that also needs to be addressed. Rosacea and eczema, for example, are known to flare with seasonal changes (11). For eczema, we want to pinpoint what their triggers are, whether those are dietary or cosmetic. There are several over-the-counter products that can help, starting with something like okra-based solutions from Zocular, and going all the way up to nonsteroidal tacrolimus-based ointments.
As the season changes, I also discuss the gut-rosacea axis. We now know that much of inflammation comes from the gut, so I talk with patients about their diet (12). The winter holidays can mean an excess of sugar, alcohol, and dairy, which can cause rosacea flares. Patients sometimes just need a reminder about the connection between what they eat and their tendency to have flares – particularly if part of their ocular surface dryness is related to skin rosacea or eczema. If they have food sensitivities, I will connect them to testing. We find a lot of undiagnosed food allergies and gut pathologies in my service.
I emphasize hydration and let patients know the importance of choosing skin products. I tell them not to be swayed by marketing and meaningless buzzwords, like “pH balanced,” “doctor recommended,” “clinically tested,” and “organic.” To be a savvy shopper, it’s all about the ingredients. The Environmental Working Group’ Skin Deep cosmetics database grades products, and I tell patients to look for products that score three and below. The Think Dirty app helps identify known irritants in products. For a deep-dive, the Tear Film and Ocular Surface Lifestyle Report on Cosmetics has great information that is easy to digest. Fragrance is a top offender, and we also want to avoid heavy preservatives. Simple is better.
Helping patients help themselves
My philosophy is "Clean, Calm, and Protect," and I find that most people can attend to these three things. If they achieve each of these goals, it’s usually sufficient to manage their condition. Every time my patients come in, I ask “How are we cleaning? How are we calming? How are we protecting?” I say this over and over again, and all patients leave my office with a specific plan on how they’re going to achieve these goals.
I also make sure patients understand that, if they’re consistent with their home care, it requires less time, less energy, and less money than pursuing other treatments. I see all of my chronic inflammatory dry patients and those with meibomian gland dysfunction or rosacea on a quarterly basis so that I know when their flares take place. Ocular surface dryness is a chronic inflammatory disease state, and it needs to be treated as such. The more compliant my patients are, the longer that they get to go in between visits.
Conclusion
To fully treat dry eye, we should recognize that it is a symptom of something deeper. This means we need to perform a thorough case history. Asking patients about their overall health can point to the root of the inflammation and a direction for therapy. Their lifestyle should be considered in order to identify anything they are putting into or on their bodies that could be exacerbating the situation. Finally, we must ensure that patients’ eyes are protected, that their lid seal is completely closed, and that they wear sunglasses when needed.
While ocular surface dryness is rarely a blinding condition, it does steal away pieces of people’s lives, bit by bit. I tell my patients that I don’t want them to be thinking about their eyes. Seasonal dry eye flares – like other inflammatory disease states that flare up – are normal and not a result of treatment failure, so I reassure patients that they are not going to regress.
References
- J Gandrup et al., “Using patient-reported data from a smartphone app to capture and characterize real-time patient-reported flares in rheumatoid arthritis,” Rheumatol Adv Pract., 6 (2022). PMID: 35392426.
- R Kapoor, YS Huang, “Gamma linolenic acid: an antiinflammatory omega-6 fatty acid,” Curr Pharm Biotechnol., 7, 531 (2006). PMID: 17168669.
- S Barabino et al., “Systemic linoleic and gamma-linolenic acid therapy in dry eye syndrome with an inflammatory component,” Cornea, 22, 97 (2003). PMID: 12605039.
- A Macrì et al, “Effect of linoleic acid and gamma-linolenic acid on tear production, tear clearance and on the ocular surface after photorefractive keratectomy,” Graefes Arch Clin Exp Ophthalmol., 241, 561 (2003). PMID: 12768289.
- P Aragona et al., “Systemic Omega-6 essential fatty acid treatment and pge1 tear content in Sjögren’s syndrome patients,” Invest Ophthalmol Vis Sci., 46, 4474 (2005). PMID: 16303936.
- KH Kokke, “Oral omega-6 essential fatty acid treatment in contact lens associated dry eye,” Cont Lens Anterior Eye, 31, 141 (2008). PMID: 18313350.
- A Pinna et al., “Effect of oral linoleic and gamma-linolenic acid on meibomian gland dysfunction,” Cornea, 26, 260 (2007). PMID: 17413949.
- F Brignole-Baudouin et al., “A multicentre, double-masked, randomized, controlled trial assessing the effect of oral supplementation of omega-3 and omega-6 fatty acids on a conjunctival inflammatory marker in dry eye patients,” Acta Ophthalmol, 89, e591 (2011). PMID: 21834921.
- JD Sheppard Jr et al., “Long-term supplementation with n-6 and n-3 PUFAs improves moderate-to-severe keratoconjunctivitis sicca: a randomized double-blind clinical trial,” Cornea, 32, 1297 (2013). PMID: 23884332.
- A Religi et al., “Estimation of exposure durations for vitamin D production and sunburn risk in Switzerland,” J Expo Sci Environ Epidemiol., 29, 742 (2019). doi: 10.1038/s41370-019-0137-2. Erratum in: J Expo Sci Environ Epidemiol., 2019. PMID: 30992519.
- V Nemeth et al., Eczema. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, Jan 2024. Last Update: March 1, 2024
- M Farshchian et al., StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, Jan 2024. Last Update: August 8, 2023.
The New Optometrist Newsletter
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Most Popular
Industry Events
Presbyopia 2024
Case Reports in Ophthalmology 2024
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here