You are viewing 1 of your 3 articles before login/registration is required
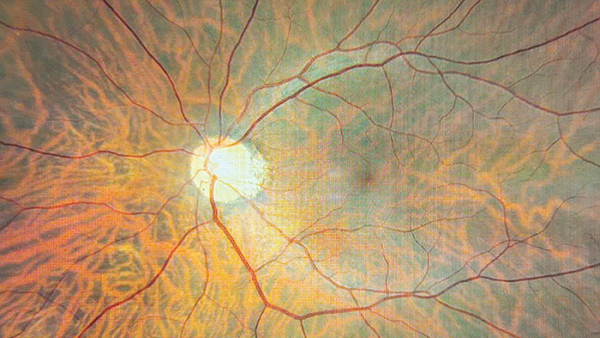
Shoring Up for the Sight Loss Tsunami
Sitting Down With… Cathy Yelf, Chief Executive, the Macular Society
When Cathy Yelf joined the Macular Society as Head of External Relations back in 2008, the charity was helping around 4000 people a year and had an income of £1.5 million. Today, with Yelf as Chief Executive, the Society helps 19,000 people and has an income of nearly £8 million. This impressive expansion notwithstanding, Yelf tells The New Optometrist that we’re only just seeing the first signs of a “tsunami of sight loss” – and the charity’s work is now more important than ever.
How did you come to work for the Macular Society?
I’d worked for the BBC for a long time, but I was getting into the later stages of my career and I thought it was time to wind down a little. A friend of mine ran the Macular Society at that time and I decided to work for him. Evidently, the winding down did not go to plan, but I’m probably the happiest I’ve ever been in a role. It’s such a rewarding field.
What was your role when you started?
I came to help with the external facing work – the communications and publicity. My job title was Head of External Relations, which makes it sound as if there was a deputy head or even a department of external relations (there wasn’t). The charity was very small at that time – and the Chief Executive had to pretty much manage the entire place.
What have been the highlights and proudest moments for you at the charity?
For me, it’s hugely important that we’ve been able to support more and more people. We have a whole range of support services, including peer support. The value of peer support really cannot be overestimated. It’s one thing to have access to experts who are well qualified and knowledgeable about eye conditions, but it’s so much more to have the kind of companionship and emotional support that ordinary people can give to each other.
There is also the increased use of digital technology. It is a complete myth that old people with macular degeneration don’t use technology! They get a great deal out of engaging with each other on their devices. I think the introduction of services that help people with technology, giving them advice on how to better use their smartphones and tablets, is another great thing we’ve achieved. And, of course, this work really took off during the pandemic, which disproportionately affected people with visual impairment.
Our involvement in medical research is also important. We know that patients value their sight more than any other sense; they fear losing their sight more than getting serious diseases, such as diabetes, and they fear it even more than losing a limb. Although we’re a small funder of eye research, we’re still one of the biggest in the sector. Next year, we will invest up to £2 million in research.
I’m also very proud that we’ve raised the profile of eye health in the last couple of years, in particular with parliamentarians and policymakers. There is a tsunami of sight loss coming towards us. We’re already in some pretty high waves, but what’s coming to shore, if we don’t invest in research into macular diseases, is very frightening. The health services cannot cope now – and yet we are probably on course for a doubling of incidents of macular disease between 2010 and 2050. Raising awareness and putting more investment into research is a very important part of the work we’ve been doing.
“Tsunami of sight loss” is an unsettling phrase to say the least… What’s driving it?
The main cause is our aging society. Age is by far the biggest risk factor for macular disease. Genetic factors account for approximately half of the risk and environmental factors, such as smoking and poor diet, contribute as well. But with so many more people living into their late eighties and nineties, the incidence will continue to rise.
Other conditions, such as glaucoma and cataract, are now being managed better as treatments are available; people with cataracts don’t go as blind as often as they used to. But that doesn’t mean sight loss is reducing. There are more people with visual impairment now than there were 25 years ago, because of the increase in conditions such as retinal disease. We also know that the number of children being diagnosed with myopia is rising very considerably. Although that isn’t a blinding disease for most people, there can be complications from myopia that develop in later life, such as myopic maculopathy.
Can you talk about the Macular Society’s recent campaigns?
We’re part of a campaign called The Eyes Have It because it’s aimed at parliamentarians. We held a very successful event in Westminster in October 2022 and 45 parliamentarians attended. Our main objective as part of The Eyes Have It is to get a national eye plan. The NHS spends hundreds of millions of pounds on eye health every year and it needs to know that the money is being spent properly. So, there needs to be a national plan; other public health problems of a similar magnitude have a national plan.
Eye health is more like dentistry than other forms of healthcare in that primary care sits outside the NHS. It’s in the high street optometry practices – the private sector. Optometry practices are not commissioned in the same way to provide comprehensive NHS services. There is a General Ophthalmic Services contract, which was a very good contract in its time, but this has not been updated to reflect the changing functions that optometry can now perform. There is more widespread use of OCT technology in optometry practices now, but in England, these new technologies are not being built into the contract. We’re not making the best use of the optometry workforce. These are not things that can be negotiated on a place-based commissioning premise. We believe they need to be negotiated nationally in the same way that the General Dental Services contract and, indeed, the GP contract is negotiated nationally.
What is the enthusiasm for a national plan from the policymakers?
After The Eyes Have It event, the health minister Will Quince tweeted that he’s heard the call for more joined-up care and will work “to bring about the positive change we all want to see.” And we have had signals from inside NHS England and other sources that a national plan would not be unwelcome.
One big thing that has changed during my time at the Macular Society is that it was almost impossible to get optometrists and ophthalmologists in the same room together 15 years ago. Now, the two professions have a much more collegiate relationship. I’m more optimistic than I was a few years ago that we can achieve a joined-up service that connects primary and secondary care. Lots of things need to be put in place first, of course. But I’m not convinced we have so much a workforce crisis as a commissioning crisis. We really need to look at commissioning so that we can make the best use of the skills we have across the pathway.
What are your priorities for the next few years?
We have three main aims. The first, of course, is to find a cure for all types of macular disease.
The second aim is to reach more people. And that means working with eye care professionals to make sure that they signpost people to our services; well-informed patients have better outcomes. More than three quarters of eye care professionals say they regularly refer patients to our services and signpost them to support charities and so on, but only about 17 percent of patients say that happens. So, there’s a disconnect between what eye care professionals are saying and what patients are hearing. We need to do a great deal more work around that to make sure that as many people as possible are able to access emotional, peer, and rehab support after diagnosis.
The third aim is to better engage political leaders, policymakers, and commissioners. We need them to fully understand the importance that people place on their vision. Yes, it helps to tell people how to look after their vision better, but we must also impress upon politicians that vision is a critical part of people’s well-being. It’s not just a “miscellaneous” concern.
The New Optometrist Newsletter
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Most Popular
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here