You are viewing 1 of your 3 articles before login/registration is required
Working at the Largest NHS Cataract Surgery Provider
Following his six-month placement at Queen Elizabeth Hospital Birmingham, Philip Wright discusses why increased volume doesn’t mean compromised care
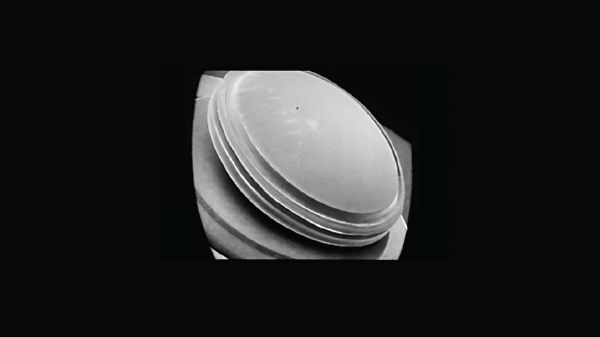
Though I started medical school with an open mind, ophthalmology felt like a natural career choice. From an early age, and owing to my mum’s work as an optometrist, I had shown an interest in the eye; it was a surgical specialty involving lots of microsurgery (which appealed to my miniature painting hobbies), and was a field at the forefront of cutting-edge technology and innovation. I also liked the fact that ophthalmology involves working with all age groups to establish a better quality of life for patients – especially with cataract surgery.
On starting at Queen Elizabeth Hospital Birmingham in 2022, my tutor offered me the opportunity to go straight into a six-month placement at SpaMedica, rather than operating at the hospital. I decided to go for it as it seemed like a great opportunity to gain experience in a different setting. I was the first trainee in our West Midlands deanery to trial such a placement.
Standard practice for trainees consists of six-monthly rotations at different hospitals within your region/deanery. In the West Midlands, during each six-month stint trainees are allocated two theater sessions per week in the hospital. The patient cases often vary – not all are cataracts, some are subspecialty specific (for example, glaucoma). If it is a theater of cataract surgery on one day, there would usually be around five or six cases on a list, but this varies from hospital to hospital.
This changes when trainees move to independent service providers, such as SpaMedica, where there are significantly higher rates of cataract cases on a list. And that’s why my placement at SpaMedica was an ideal stepping stone for my stage of training. I had already treated approximately 60 cataracts independently and wanted experience in a greater number of cases – which is exactly what I got. I slowly built up my skills and confidence to be able to perform 16 cases in a full day. In total, I treated 190 cases in six months, operating one full day per week.
I’d been advised by my tutor to observe how the way of working was different in a high-volume environment such as that found in SpaMedia, and to notice how patient flow and various other factors differed from my previous theater experiences. For me, this was just as interesting as the surgery – the much quicker patient turnaround times, the space available for preparation, and even having a staff member on hand to sort out the operation notes. All of these things made high-volume surgery achievable; all I had to do was concentrate on the patient and the surgery itself. And so, despite the higher volumes, there was never a feeling of being rushed for time whilst I was training. Efficiency was part of the job; the faster turnover between each case was made possible due to excellent support from theater staff.
The team at SpaMedica Birmingham were exceptionally welcoming and supportive of me. My clinical supervisor, Kenan Damer, was kind and patient; he gave fantastic constructive feedback that I could immediately implement, and encouraged me to do as many cases as I could comfortably manage. My timings improved week on week under his guidance, so I was able to complete the list independently as I got towards the end of the placement.
Importantly, the volume of cases in no way impacted the quality of care each patient received. Patients were sometimes very anxious ahead of their surgery, and the team would always go above and beyond to help them feel as calm, settled, and as looked after as possible. Everyone would pitch in, ensuring patients were comfortable, help them with their positioning, hold their hands, assist them in transferring and so on.
Patients were positive about my training too. Damer would reassure them if there were any initial doubts. He would say that he fully trusted me as a surgeon and that he was on hand to supervise if needed.
I operated on a range of complex cataract cases, including small pupils, shallow anterior chambers, dense cataracts, patients with previous refractive surgery, diabetes, Parkinsonian tremors, corneal opacities, and more. I now feel able to approach any case and adapt to it appropriately. And I’m proud of the outcomes I achieved: my PCR rate was 0.7 percent – well below the national benchmark of 1.1 percent (SpaMedica’s unadjusted PCR rate is 0.49 percent) and all patients I treated achieved a visual acuity score of 6/12 or better, regaining driving standard vision after surgery.
I believe there’s a balance to be found in independents like SpaMedica continuing to support the NHS to cut waiting times and improve patient outcomes and experiences. Once I’ve completed my training, I hope to split my work between both public and independent sectors. And I now feel equipped with the skills I need to manage my own high-volume theater list – whatever the setting.
This article first appeared in The Ophthalmologist
The New Optometrist Newsletter
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Most Popular
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here