You are viewing 1 of your 3 articles before login/registration is required
New Frontiers: The Quest for Pan-Ocular Imaging
Why navigated SS-OCT and pan-retinal imaging have revolutionized the diagnosis of vitreoretinal diseases and can change referral patterns and management
Over the past few decades, there has been a significant increase in our understanding of vitreous and retinal diseases, thanks to advances in retinal imaging techniques – now essential tools for both ophthalmologists and optometrists. Standard fundus imaging systems – which provide a 30–60° field of view of the retina – have given way to the widefield (WF) and ultra-widefield (UWF) imaging devices that are also becoming commonplace in clinical practice (1).
There are some inconsistencies, however, in the use of different terminology when describing these imaging techniques that can be misleading and confusing. It is recommended that optometrists and ophthalmologists follow the International Widefield Imaging Study Group’s consensus on defining these terms. The term WF is limited to single images, and not montages, depicting retinal anatomic features beyond the posterior pole but posterior to the four vortex vein ampullas. Whereas retinal images showing anatomic features anterior to these ampullas can be called UWF (2).
Moreover, some UWF imaging devices, such as the Optos Silverstone, have the potential to combine several imaging modalities (multimodal imaging), including red/green (RG), fundus autofluorescence (FAF), fundus fluorescein angiography (FFA), and indocyanine green angiography (ICGA) imaging. In addition, this device has the capability of performing these imaging modalities simultaneously with navigated central and peripheral swept source optical coherence tomography (SS-OCT).
All imaging devices have different capabilities and benefits to assess central and peripheral vitreoretinal and choroidal abnormalities.
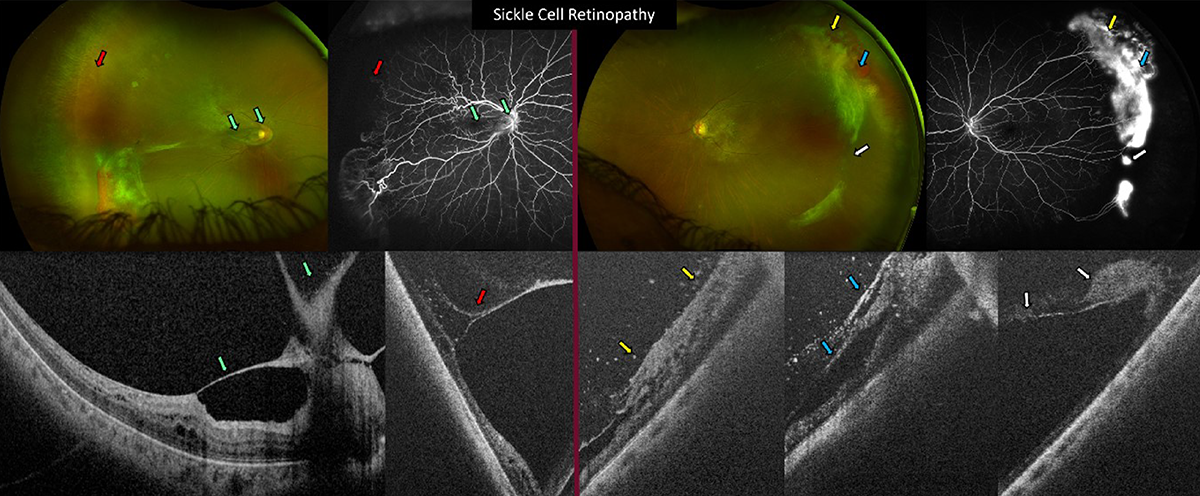
Figure 1: Sickle cell retinopathy.
OD: A typical sea-fan neovascularization observed with ultra widefield red/green (UWF RG) and UWF fundus fluorescein angiography (FFA). Vitreomacular traction, a thickened internal limiting membrane (ILM) and intraretinal fluid (macular oedema) were observed using macular SS-OCT scans over UWF FFA which showed traction-induced vascular distortion with shortening of the distance between the posterior pole temporal vascular arcades (green arrow). Peripheral navigated SS-OCT over UWF FFA demonstrated vitreoretinal traction on sea-fan neovascularization with intraretinal fluid and schitic changes as well as traction-induced vascular distortion (red arrow).
OS: Peripheral navigated SS-OCT over UWF RG and UWF FFA of the fellow eye also showed vitreoretinal traction on sea-fan neovascularization with red blood cells in the cortical vitreous, retinal schitic changes as well as traction-induced vascular distortion on peripheral retina (yellow, blue and white arrows).
OCT on the up
Since its advent in 1991, OCT has evolved at an impressive rate and is now arguably the most important imaging technique in ophthalmology (3–8). The advantages of SS-OCT include high scanning speed, deeper penetration, no loss of sensitivity across the image from the vitreous up to the inner surface of the sclera, and better visibility through opaque media. However, most commercially available OCT scanners can only image within the posterior pole due to their limited field of view.
In 2021, I was part of a team that demonstrated the feasibility of navigated single-capture cross sectional and 3D SS-OCT imaging, which provides detailed anatomic information, allowing for early recognition of vision-threatening features that influence the clinical management (9).
Navigated SS-OCT imaging has revolutionized peripheral imaging because of its capability to allow for cross-sectional, en face, and 3D-rendering images of the mid and far periphery.
The rest of the team and I strongly believe that this imaging technology can change the approach to diagnosing and treating many retinal diseases.
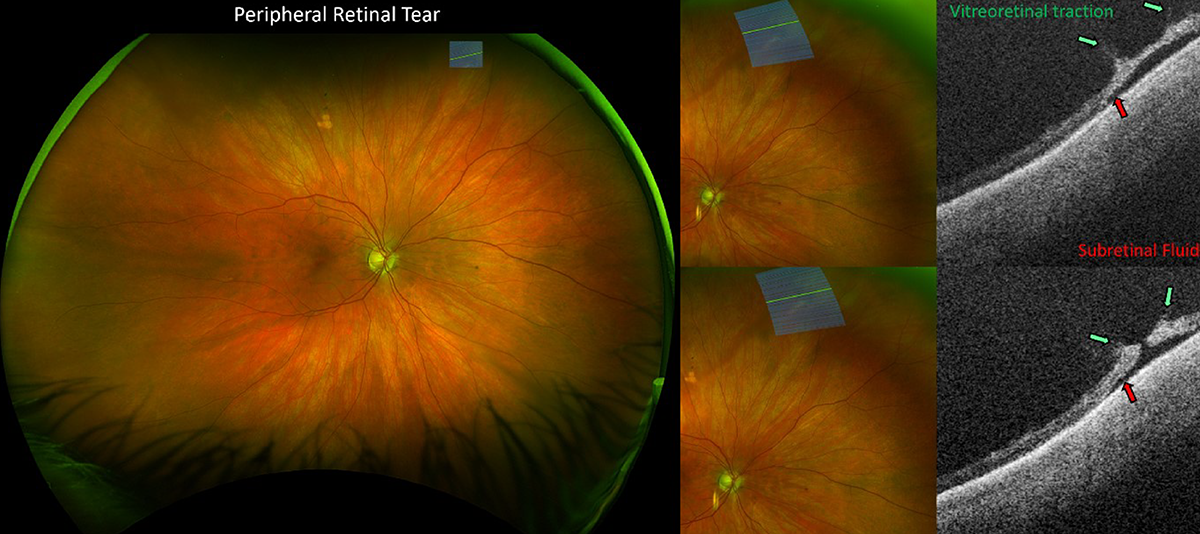
Figure 2: Peripheral retinal tear.
Ultra widefield red/green (UWF RG) imaging showed a right eye superonasal extremely peripheral retinal round hole. Navigated peripheral cross-sectional SS-OCT showed vitreoretinal traction (green arrows) and subretinal fluid (red arrows) not visible on ophthalmoscopy.
A panretinal approach
Embryologically, the central portion of the neuroretina differentiates early, while the cells in the peripheral retina remain proliferative, which allows for signs of ocular and systemic diseases to develop in different areas of the retina (10). Ultra-widefield and peripheral navigated SS-OCT imaging may therefore help us to better understand such peripheral manifestations and allow for early diagnosis with less invasive and more successful management. In addition, this will allow for a change in the assessment of “only macular diseases”, precursors of which may be detected in the peripheral retina before being detected in the central retina. In other words, we may address such diseases as panretinal.
Floaters be gone!
In addition to the peripheral retina, eye care specialists are focusing more on vitreous pathologies. Vitreous floaters are a growing problem because of the evolving global incidence of myopia and more demanding visual requirements (11,12). Floaters can be perceived as extremely bothersome and can be challenging to live with (8). However, treatment is often ignored as floaters are not always visible to the examiner. We also do not yet have enough understanding of the correspondence between subjective symptoms and objective data.
I believe there is a need for imaging techniques that can lead to a better understanding of patients’ symptoms and the impact of floaters on their vision. Navigated UWF imaging techniques with deeper scan depth capability are helping to better visualize vitreous anatomy, allowing eye care practitioners to visualize bothersome floaters and be able to objectively manage patients’ conditions.
We have recently introduced the new terminology of Vitreous Floaters and Opacities (VFO), which we believe more accurately describes the symptoms reported by patients and their appearance on imaging, and the results of the first objective and standardized test that takes into account their kinesis and intermittent effect on vision.
Our newly proposed SK VFO Test provides insight into the type of VFO and severity of symptoms and has the potential to personalize the management of VFO and define eligibility criteria for either full or limited vitrectomy surgery, combined with or without phacoemulsification or Nd-YAG vitreolysis (13).
The use of standardized and kinetic tests in subjects with symptoms provides additional insights into the type of floaters and severity of symptoms (considering characteristics such as number, dimensions, opacity, movement, and latency of the floaters). This standardization is also essential to individualize the treatment of floaters, either with YAG laser vitreolysis or limited pars plana vitrectomy (14,15).
Objectivity in PVD diagnosis
Finally, it is important to be able to objectively establish posterior vitreous detachment (PVD) status in order to determine risks in the symptomatic and in the fellow eye, even if asymptomatic.
Diagnosis of PVD is not standardized and differs widely in most published series. PVD is usually difficult to diagnose in the absence of a visible Weiss Ring and scenarios like the presence of vitreous schisis can lead to an erroneous diagnosis of PVD.
It is therefore important to counsel patients based on objective imaging-based evidence of PVD status and we believe that widefield, central and navigated peripheral SS-OCT imaging are essential for the objective diagnosis of the PVD status (8, 9).
Regardless of the advances in imaging, indirect ophthalmoscopy with 360 degree scleral indentation is still essential for a complete examination of the vitreoretinal interface and retina up to the ora serrata.
These novel imaging technologies and techniques yield additional quantitative and qualitative evaluation, which contributes to a better understanding of abnormalities. Such information can then be used for objective monitoring, establishing the need and timing of referrals and for a well-informed discussion of available treatment options prior to the referral.
In conclusion, vitreous, navigated OCT and ultra-widefield imaging are the current “gold standard.” They are better suited for the screening, early diagnosis, and monitoring of vitreoretinal conditions, as well as for use in telemedicine and artificial intelligence. We strongly believe that we will see significant advances in this field of imaging over the next five years and as part of our quest to achieve single-scan pan-ocular imaging.
References
- M Fogel-Levin et al., “Advanced retinal imaging and applications for clinical practice: A consensus review,” Survey of Ophthalmology, 67 1373–1390 (2022).
- N Choudhry et al., “Classification and guidelines for widefield imaging: recommendations from the international widefield imaging study group,” Ophthalmol. Retina, 3, 843–849 (2019).
- PE Stanga, AC Bird “Optical coherence tomography (OCT): principles of operation, technology, indications in vitreoretinal imaging and interpretation of results,” Int. Ophthalmol., 23, 191-197 (2001).
- PE Stanga et al., “Swept-source optical coherence tomography angio™ (Topcon Corp, Japan): technology review,” Dev. Ophthalmol., 56, 13-17 (2016).
- MM Muqit et al., “Optos-guided pattern scan laser (Pascal)-targeted retinal photocoagulation in proliferative diabetic retinopathy, Acta. Ophthalmol., 91, 251-258 (2013).
- PE Stanga et al., “Comparison of optical coherence tomography and fluorescein angiography in assessing macular edema in retinal dystrophies: preliminary results,” Int. Ophthalmol. 23, 321-5 (2001)
- D Huang, “Optical coherence tomography,” Science, 254, 1178–1181 (1991)
- PE Stanga et al., “In vivo imaging of cortical vitreous using 1050-nm swept-source deep range imaging optical coherence tomography,” Am. J Ophthalmol. 157, 397-404 (2014).
- PE Stanga et al., “Navigated single-capture 3D and cross-sectional wide-field OCT of the mid and peripheral retina and vitreoretinal interface,” Eur. J Ophthalmol., 32, 1642–1651 (2022).
- N Quinn et al., “The clinical relevance of visualizing the peripheral retina,” Prog. Retin. Eye Res., 68, 83–109 (2019).
- BA Holden et al., “Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050,” Ophthalmology, 123, 1036–1042 (2016).
- JH Nguyen et al., “Vitreous structure and visual function in myopic vitreopathy causing vision-degrading myodesopsia,” Am. J Ophthalmol., 224, 246–253 (2021).
- PE Stanga et al. (in press), “New terminology and methodology for the assessment of the vitreous, its floaters and opacities, and their effect on vision: standardized and kinetic anatomical & functional testing of VFO (vitreous floaters and opacities) (SK VFO Test), Ophthalmic Surg. Lasers Imaging Retina (2023).
- PE Stanga, D Reinstein, “Managing vision degrading myodesopsia (VDM): assessment of the vitreoretinal interface (VRI) and vitreous opacity (VO), intra-laser videos and first year results using YAG laser vitreolysis (YLV),” Poster presentation, Jules Gonin Meeting 2020.
- DD Dysager et al., “Efficacy and safety of pars plana vitrectomy for primary symptomatic floaters: a systematic review with meta-analyses,” Ophthal. Ther., 11, 2225–2242 (2022).
The New Optometrist Newsletter
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here
Sign up to The New Optometrist Updates
Permission Statement
By opting-in, you agree to receive email communications from The New Optometrist. You will stay up-to-date with optometry content, news, events and sponsors information.
You can view our privacy policy here